Prediabetes Is More Common Than You Think—Here Are 14 Signs to Watch Out For

Prediabetes can feel frustratingly invisible, because many people don’t notice anything “wrong” until their numbers are already trending high.
Still, your body may drop hints when blood sugar control is starting to slip and insulin resistance is building in the background.
The tricky part is that these signs are easy to blame on stress, getting older, a busy schedule, or not sleeping enough, which is why they often get brushed off for months (or years).
If a few of these symptoms sound familiar—especially if they’re new, persistent, or happening together—it’s worth bringing up with your doctor and asking about a simple screening such as an A1C or fasting glucose test.
Catching prediabetes early can make a big difference, because small changes are often enough to steer things back in a healthier direction.
1. You’re thirsty all the time (even when you’re drinking plenty of water)

Needing water more than usual can be one of those subtle changes you chalk up to weather, exercise, or salty food, but it may also be your body’s way of coping with higher-than-normal blood sugar.
When glucose builds up in the bloodstream, your kidneys work harder to filter and flush the excess, and that process pulls more fluid from your tissues.
As a result, you may feel persistently dry-mouthed, crave cold drinks, or notice that you’re refilling your bottle far more often than you used to.
The pattern matters, too: thirst that’s frequent, intense, and not relieved by normal hydration deserves attention.
If it’s paired with other changes like increased urination or fatigue, it’s a good idea to get your blood sugar checked rather than assuming it’s “just dehydration.”
2. You’re peeing more often than usual, including waking up at night

A sudden increase in bathroom trips can be more than a nuisance, particularly when it starts interrupting sleep.
One reason this can happen is that the body tries to get rid of extra glucose through urine, which means the kidneys pull more water into that process.
You might notice larger amounts of urine, more frequent urges, or waking up in the middle of the night when you used to sleep straight through.
While lots of things can cause this—like drinking more caffeine, a urinary tract infection, or certain medications—frequent urination that lingers for weeks is worth discussing with a clinician.
Paying attention to timing helps: if nighttime trips become routine and you’re also thirstier than normal, that combination can be a meaningful clue that blood sugar regulation isn’t as steady as it should be.
3. You feel unusually tired or drained—even after a decent night’s sleep
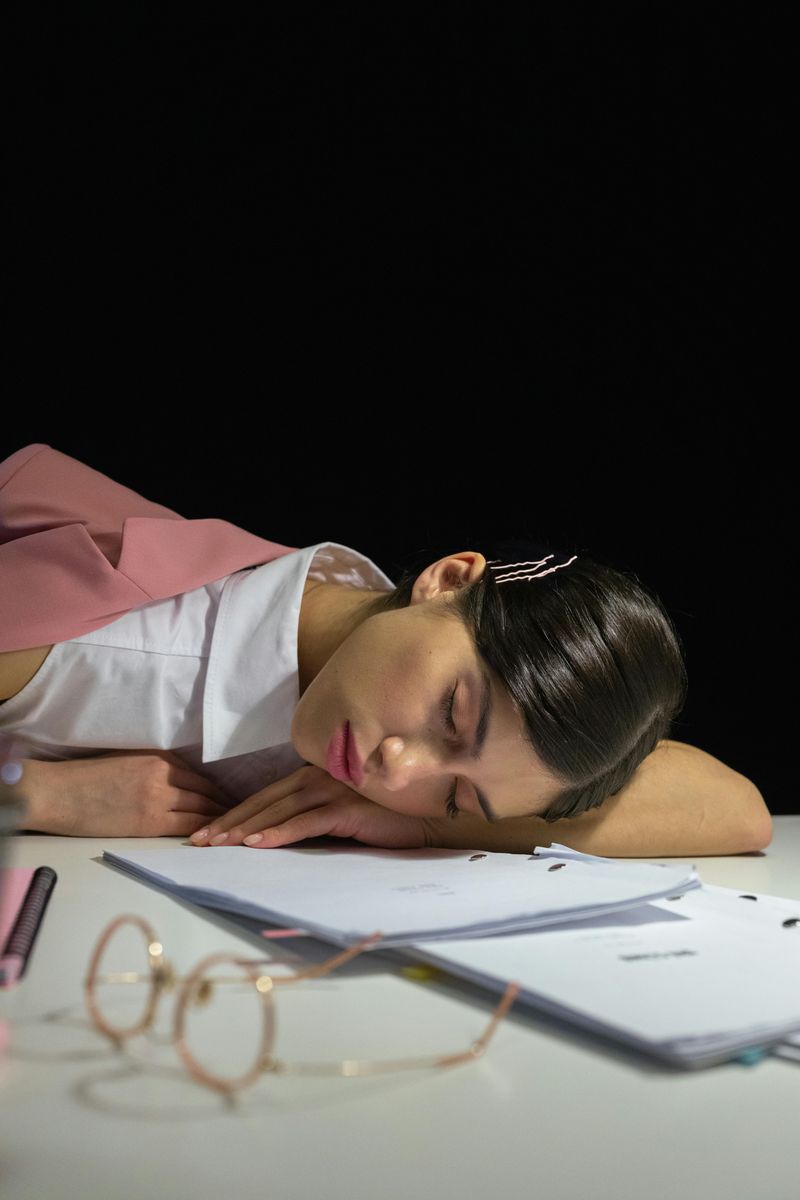
Feeling worn out can be normal in a busy season of life, but persistent exhaustion can also be a sign your body isn’t using energy efficiently.
When insulin resistance is developing, glucose may have a harder time getting into cells where it can be used for fuel, which can leave you feeling strangely drained even if you’ve eaten and slept “normally.”
You may notice afternoon crashes, a heavy, sluggish feeling after meals, or a sense that your energy never fully rebounds no matter how early you go to bed.
This kind of fatigue can be especially confusing because it often overlaps with stress, anemia, thyroid problems, and burnout.
That’s why it helps to look at the full picture: if the tiredness is new, consistent, and paired with thirst, frequent urination, or brain fog, it’s smart to rule out blood sugar issues.
4. You get “hangry” fast or feel shaky/lightheaded between meals

Some people notice they don’t simply get hungry; they get irritable, jittery, or suddenly weak if they go too long without eating.
This can happen when blood sugar rises and falls in a more dramatic pattern than your body prefers, which may be linked to insulin resistance and the way your system handles carbs.
You might feel fine after breakfast, then become shaky by late morning, or you may experience a sudden mood shift that improves quickly once you eat.
While true low blood sugar is more common in people taking certain diabetes medications, swings can still feel uncomfortable in prediabetes, especially after high-sugar meals followed by a long gap.
Keeping track of when it occurs can be revealing.
If symptoms show up repeatedly a couple of hours after eating—especially carbs-heavy snacks—it’s worth asking about blood sugar testing and focusing on balanced meals with protein and fiber.
5. Brain fog (you can’t focus like you used to)

Concentration issues can feel like a personality change when you’re used to being sharp and organized.
Fluctuating blood sugar may contribute to that foggy sensation, because the brain is sensitive to changes in available energy and hydration.
You might notice you’re rereading the same email, forgetting why you walked into a room, or struggling to stay focused during tasks that used to be easy.
This isn’t the same as occasional distraction; it often feels like your mind is wading through mud, especially after meals or on days when you’re also feeling tired.
Of course, brain fog can come from lack of sleep, anxiety, hormonal shifts, or even dehydration, so it’s not a stand-alone diagnosis.
Still, if it’s persistent and paired with increased thirst, frequent urination, or unusual hunger, checking your glucose numbers can help you understand whether blood sugar instability is part of the story.
6. Blurred vision that comes and goes

Vision changes aren’t always about needing a new prescription, especially when the blur appears suddenly and then clears up later.
Shifts in blood sugar can affect fluid levels in the body, including inside the eyes, which may temporarily change the shape of the lens and alter focus.
That can make text look slightly fuzzy, lights appear hazier, or your eyes feel strained after reading.
Intermittent blur can be easy to dismiss, because it’s not constant and might seem related to screen time or tiredness.
However, if the changes happen repeatedly—especially along with thirst, frequent urination, or fatigue—it’s worth mentioning to a healthcare professional.
Eye symptoms don’t automatically mean diabetes, but they can be a sign that glucose levels are fluctuating enough to influence vision.
The sooner you catch that pattern, the sooner you can address what’s driving it.
7. Increased hunger—especially cravings for carbs/sweets

A shift in appetite can show up quietly, like feeling unsatisfied after meals that used to keep you full, or thinking about snacks far more often than normal.
When insulin resistance is developing, cells may not access glucose as effectively, which can send your body signals that it needs more fuel even if you’ve eaten recently.
That can lead to persistent hunger and cravings for quick energy sources like bread, sweets, or sugary drinks.
The frustrating part is that giving in often creates a cycle: a carb-heavy snack can spike blood sugar, followed by a crash that makes you hungry again.
Many people interpret this as a lack of willpower, but it can be partly biological.
If you’re noticing a new pattern of strong cravings, frequent snacking, or feeling “starving” soon after meals, it’s worth checking your blood sugar and experimenting with more protein, fiber, and healthy fats for steadier satisfaction.
8. Slow-healing cuts, scrapes, or bruises

Healing speed can offer clues about what’s happening internally, even when the injury seems minor.
When blood sugar runs higher than ideal, it can interfere with circulation and immune response, which are both important for repairing tissue.
You might notice that small cuts stay red longer, a blister takes forever to close up, or bruises linger for days beyond what feels normal for you.
This doesn’t mean every slow-healing scab is a medical emergency, but a noticeable change in how your body recovers is worth paying attention to.
It can be especially telling when combined with frequent infections or skin issues.
The good news is that identifying the cause early can help you protect your health long term.
If you keep thinking, “Why is this taking so long to heal?” it’s a smart moment to ask your doctor about blood sugar screening, along with other common contributors like anemia or nutrient deficiencies.
9. More frequent infections (like UTIs, yeast infections, or skin infections)

When infections start popping up more often than usual, it can feel like bad luck, but blood sugar can play a role.
Higher glucose levels can create an environment where bacteria and yeast thrive, particularly in warm, moist areas of the body.
Some people notice recurring urinary tract infections, more frequent yeast infections, or irritated skin that becomes infected more easily.
This can be especially frustrating because the problem may keep returning even after treatment, making it feel like you can’t get ahead of it.
Of course, recurring infections can have many causes—hormonal changes, antibiotics, immune issues, or even certain birth control methods—so it’s not a definitive sign on its own.
Still, if infections are becoming a pattern and you’re also dealing with thirst, fatigue, or increased urination, it’s worth considering blood sugar testing as part of the bigger picture rather than treating each episode in isolation.
10. Tingling or numbness in hands/feet (can happen as blood sugar affects nerves)

Odd sensations like pins-and-needles, mild burning, or numbness in your toes can be easy to shrug off as poor posture or sleeping “wrong,” but nerve irritation can also be related to blood sugar changes.
Over time, elevated glucose can affect small nerves and blood vessels, which may contribute to tingling in the extremities even before diabetes is diagnosed.
Some people notice it more at night, while others feel it after sitting for a while.
It’s important not to self-diagnose here, because tingling can also come from vitamin B12 deficiency, thyroid issues, back problems, or carpal tunnel syndrome.
The key is persistence and pattern: if the sensation keeps returning, spreads, or becomes more noticeable alongside other prediabetes clues, it’s worth bringing up at an appointment.
Early evaluation matters, because addressing blood sugar and other contributing factors can help prevent progression and reduce discomfort over time.
11. Dark, velvety patches of skin on the neck, underarms, or groin (often linked with insulin resistance)

Changes in skin texture and color can be one of the more visible clues tied to insulin resistance.
A common example is a darkened, slightly thickened “velvety” area that shows up on the back of the neck, under the arms, or in the groin area.
This condition is often called acanthosis nigricans, and it can look like a patch that won’t wash off, even with exfoliating.
People sometimes assume it’s dirt, irritation from shaving, or a reaction to deodorant, but it can be linked to higher insulin levels circulating in the body.
That doesn’t automatically mean diabetes, but it’s worth taking seriously as a prompt to ask about metabolic health and blood sugar.
If you notice these patches developing or spreading, consider it a helpful warning sign rather than a cosmetic issue.
Checking A1C and discussing insulin resistance with a clinician can clarify what’s going on and what to do next.
12. Skin tags showing up more often (commonly around the neck/underarms)

Skin tags are common and usually harmless, but a noticeable increase can sometimes show up alongside insulin resistance.
These small, soft growths often appear where skin rubs—like the neck, underarms, eyelids, or under the breasts—and they can be easy to ignore because they’re not painful.
Still, when multiple new tags appear over a short period, it can be a useful clue to look at the bigger health picture rather than treating them as random.
Researchers have noted associations between skin tags and metabolic changes, including higher insulin levels, which is why doctors sometimes consider them a subtle flag for prediabetes risk.
Of course, friction, genetics, and weight changes can also contribute, so it’s not a diagnostic sign by itself.
However, if skin tags are increasing and you’re also noticing fatigue, cravings, or frequent urination, it’s reasonable to ask for blood sugar screening and discuss lifestyle changes that support insulin sensitivity.
13. Unexplained weight gain around the belly (or difficulty losing weight despite trying)

Body changes can feel discouraging when you’re doing “the right things” and nothing seems to move, but insulin resistance can make weight management harder.
Higher insulin levels can encourage the body to store fat, particularly around the abdomen, and some people find they gain weight even without a major change in diet.
Others don’t gain much but struggle to lose weight despite consistent effort.
This can create a frustrating cycle, because the harder you push with extreme dieting, the more cravings and energy crashes can follow.
While many factors influence belly weight—stress hormones, sleep quality, menopause, and thyroid function among them—persistent central weight gain can be one more clue to evaluate blood sugar and metabolic health.
Paying attention to waist measurements, not just the scale, can be helpful.
If you feel like your midsection changed quickly or weight loss has become unusually difficult, it’s worth asking about an A1C test and focusing on sustainable habits like strength training, fiber-rich meals, and consistent sleep.
14. Mood changes—irritability, anxiety, or feeling “off” when you haven’t eaten

Emotional shifts can be a surprisingly physical issue when blood sugar is unstable.
Some people notice they feel anxious, short-tempered, or unusually sensitive when they go too long without food, and then feel like themselves again after a balanced meal.
That can happen when glucose levels spike and drop more dramatically, which can affect energy, stress hormones, and overall comfort.
It’s easy to write this off as stress or being “too busy,” but patterns matter.
If you’re consistently snapping at people before lunch, feeling edgy late afternoon, or getting hit with an emotional wave that seems to come out of nowhere, it may be worth considering how your meals are structured.
A breakfast that’s mostly carbs, for example, can leave you feeling shaky later.
While mood changes aren’t exclusive to prediabetes, they can pair with other signs like cravings, fatigue, and brain fog.
Tracking when the irritability hits and discussing it with your doctor can help identify whether blood sugar swings are playing a role.

Comments
Loading…