Feeling Off? These 21 Everyday Signs Could Be Related to Inflammation

Inflammation is your body’s natural response to injury and infection, but when it lingers silently, it can cause serious health problems down the road. Many of us experience subtle warning signs of chronic inflammation without realizing what they mean. Recognizing these early signals gives you a chance to make changes before inflammation leads to bigger health issues.
1. Brain Fog That Won’t Lift

Your once-sharp mind now feels wrapped in cotton. Words escape you mid-sentence, and simple tasks require extra concentration. This mental cloudiness isn’t just stress or aging—it’s often your brain responding to inflammatory messengers circulating in your bloodstream.
These inflammatory compounds can cross the blood-brain barrier, affecting how your neurons communicate. The result is sluggish thinking, forgetfulness, and difficulty focusing that persists regardless of how much coffee you drink or sleep you get.
Many people notice improvement when they identify their inflammatory triggers, whether they’re dietary (like sugar or processed foods), environmental, or stress-related. Addressing these root causes often clears the mental haze faster than any brain-training app.
2. Mood Swings That Surprise You

Suddenly snapping at loved ones over minor issues? Your unexpected irritability might have inflammatory roots. When inflammatory molecules circulate in your bloodstream, they don’t just affect your joints—they change your brain chemistry too.
Research shows that inflammation disrupts the production and regulation of mood-stabilizing neurotransmitters like serotonin and dopamine. This biochemical imbalance can trigger emotional responses that feel disproportionate even to you as you’re experiencing them.
The connection is so strong that some researchers now view certain types of depression as inflammatory disorders. If your emotional thermostat seems broken, looking for sources of inflammation—from diet to chronic stress—might provide more relief than willpower alone.
3. Anxiety That Appears Without Reason

That feeling of dread settling over you for no apparent reason might be your body’s inflammatory alarm system. Researchers have discovered that inflammatory cytokines can directly affect the areas of your brain responsible for fear and anxiety responses.
Many people describe this inflammation-driven anxiety as feeling “wired but tired”—simultaneously exhausted yet unable to relax. Your body is essentially stuck in a low-grade fight-or-flight response, even when no immediate threat exists. What makes this particularly confusing is that the anxiety often doesn’t connect to specific worries or thoughts.
It’s more of a physical sensation of unease that your mind then tries to attach to something concrete. Anti-inflammatory approaches often help where traditional anxiety management falls short.
4. Fatigue That Sleep Can’t Fix

Eight hours of sleep should leave you refreshed, but you’re still dragging yourself through the day. This bone-deep exhaustion that no amount of rest seems to cure often signals inflammatory processes working overtime in your body.
When your immune system is chronically activated, it diverts energy away from normal cellular functions. Your mitochondria—the powerhouses within your cells—become less efficient at producing energy when inflammation persists. The result is a profound fatigue that differs from normal tiredness.
Many people describe it as feeling like they’re “moving through molasses” or “carrying a heavy backpack” through daily activities. If extra sleep and cutting back on commitments doesn’t restore your energy, investigating inflammatory triggers might uncover the real energy thief.
5. Restless Nights and Broken Sleep

Tossing and turning has become your nightly routine, despite feeling exhausted. This frustrating sleep disruption often stems from inflammatory messengers interfering with your brain’s sleep-regulating mechanisms. Inflammation alters your production of melatonin (your sleep hormone) and affects your circadian rhythm—the internal clock that governs when you feel alert or sleepy.
Your body temperature regulation, another crucial aspect of quality sleep, gets thrown off by inflammatory processes. The relationship works both ways: poor sleep increases inflammation, and inflammation disrupts sleep.
Breaking this cycle often requires addressing the underlying inflammatory triggers rather than just trying conventional sleep remedies. Many people notice that anti-inflammatory dietary changes improve their sleep quality before other symptoms.
6. Morning Joint Stiffness That Fades After Moving

Your first steps out of bed feel like you’re 90 years old, but by breakfast time, you’re moving normally again. This temporary morning stiffness that improves with movement is a classic early warning of inflammatory processes targeting your joints.
During sleep, inflammatory fluid can accumulate in joint spaces when you’re not moving. The immobility allows inflammatory compounds to concentrate, creating that characteristic stiffness that decreases as you get moving and circulation improves. If this lasts less than 30 minutes, it’s typically considered mild. Don’t dismiss this symptom just because it goes away!
This pattern often precedes more serious inflammatory joint conditions by months or years. Catching and addressing it early can prevent progression to more persistent problems that don’t resolve with simple movement.
7. Muscle Aches Without Obvious Cause

Your muscles feel sore and tender, but you haven’t hit the gym or done anything strenuous. This mysterious achiness that appears without exertion often signals that inflammatory markers like C-reactive protein are elevated in your system.
Unlike the satisfying soreness after a good workout, inflammation-related muscle pain tends to be more diffuse and persistent. It commonly affects larger muscle groups and may be accompanied by a feeling of weakness or heaviness in the limbs. Many people describe it as feeling like they’re coming down with the flu, except the feeling never fully develops into illness.
This type of muscle discomfort often fluctuates with stress levels, diet, and sleep quality—all factors that influence your body’s inflammatory state. Tracking these variables can help identify your personal inflammation triggers.
8. Bloating After Normal Meals

Your stomach swells up after eating ordinary portions of food, making you look several months pregnant by evening. This disproportionate bloating often indicates inflammation in your digestive tract, particularly in the intestinal lining.
When your gut becomes inflamed, even slightly, it affects how efficiently you digest food and how quickly it moves through your system. Gas-producing bacteria may proliferate, and your intestinal muscles may not contract properly. The result is trapped gas, slowed digestion, and that uncomfortable distended feeling.
Many people mistakenly attribute this symptom solely to specific foods, when it’s actually the underlying inflammation making their digestive system hypersensitive. Addressing gut inflammation often allows greater dietary flexibility as the digestive tract becomes more resilient and less reactive.
9. New Food Sensitivities Appearing

Foods you’ve enjoyed your entire life suddenly leave you feeling unwell. This adult-onset food sensitivity phenomenon often indicates that inflammation has compromised your gut barrier, creating what some health professionals call “leaky gut.”
When inflammation damages the tight junctions between intestinal cells, partially digested food particles can enter your bloodstream, triggering immune responses. Your body essentially starts treating harmless foods as invaders. Common culprits include gluten, dairy, eggs, and soy, but reactions can develop to virtually any food.
The confusing part is that reactions may be delayed by hours or even days, making connections difficult to spot without systematic tracking. Addressing the underlying gut inflammation often allows some food tolerance to return, rather than requiring permanent elimination of more and more foods.
10. Blood Sugar Crashes and Intense Cravings

Mid-afternoon energy crashes leave you desperately hunting for sugar or caffeine. These dramatic blood sugar fluctuations often signal that inflammation is interfering with your insulin sensitivity and glucose metabolism. When inflammatory compounds are circulating in your bloodstream, they can block insulin receptors on your cells.
This creates a situation where your pancreas pumps out plenty of insulin, but your cells can’t properly respond to it. The result is blood sugar that swings wildly rather than maintaining steady levels. These crashes trigger intense cravings as your brain, sensing the energy crisis, drives you toward the quickest fuel sources. Unfortunately, giving in to these cravings perpetuates the inflammatory cycle.
Many people break this pattern by focusing on anti-inflammatory foods that stabilize blood sugar rather than fighting willpower battles.
11. Skin Rashes That Come and Go

Mysterious red patches appear on your skin without any change in products or environment. These unexplained rashes often represent your skin—your largest organ—reflecting internal inflammatory processes happening elsewhere in your body. Your skin contains immune cells that respond to inflammatory signals circulating in your bloodstream.
When inflammation becomes systemic, these skin-based immune cells can become activated even without direct skin contact with an irritant. The resulting rashes may appear as redness, small bumps, or dry, flaky patches that seem to migrate around the body.
Pay attention to timing—many people notice these rashes flare after consuming inflammatory foods or during periods of high stress. The skin often serves as an early warning system for internal inflammation before more serious symptoms develop in less visible organs.
12. Facial Puffiness, Especially Around Eyes

Morning mirror checks reveal a puffy face that doesn’t match last night’s salt intake. This subtle swelling, particularly noticeable around the eyes and jawline, often indicates inflammatory fluid retention throughout your body. When inflammation is present, your capillaries become more permeable, allowing fluid to leak into surrounding tissues.
This process, called edema, is especially noticeable in areas with thin skin and loose connective tissue—like your eyelids and under-eye area. The result is that slightly swollen, tired appearance that makeup can’t quite disguise. While many people blame poor sleep alone for this symptom, addressing inflammatory triggers often reduces facial puffiness more effectively than extra rest.
Morning face puffiness that consistently appears regardless of sleep quality deserves attention as a potential inflammation warning sign.
13. Hair Thinning or Texture Changes
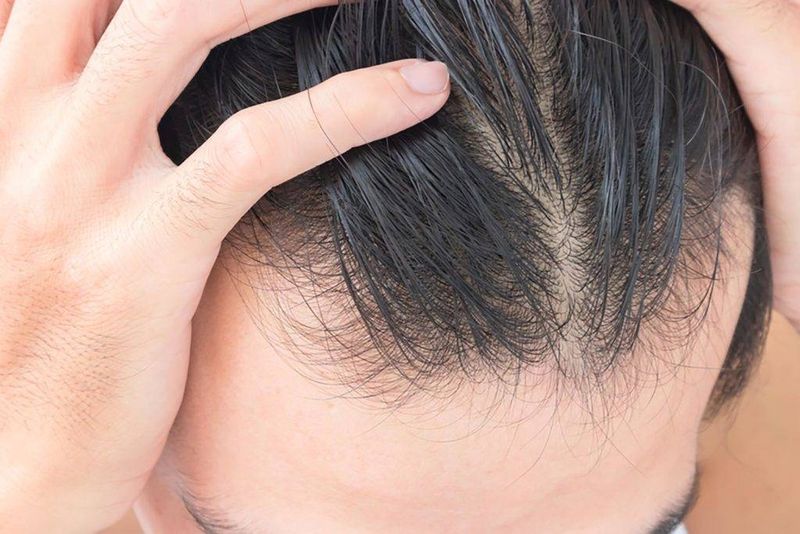
Your once-thick locks are becoming noticeably thinner, or your hair texture has changed for no apparent reason. These changes often indicate that inflammation is affecting your hair follicles and disrupting normal growth cycles. Hair follicles are among the body’s most metabolically active tissues, making them highly sensitive to inflammatory signals and reduced circulation.
When inflammation is present, hair follicles can prematurely enter their resting phase, leading to increased shedding without proper replacement. The inflammation also affects the quality of new hair growth, altering texture, shine, and strength.
While many attribute hair changes solely to aging or hormones, addressing underlying inflammation often improves hair quality more effectively than topical treatments alone. Your hair essentially serves as a visible barometer of your internal inflammatory environment.
14. Frequent Colds That Linger

You catch every bug going around, and what should be a quick cold turns into weeks of sniffles. This compromised immune response often indicates that your immune system is preoccupied with chronic inflammation elsewhere in your body.
When your immune resources are diverted to address persistent low-grade inflammation, your ability to mount an effective defense against new invaders becomes compromised. It’s like having your security forces already deployed, leaving your borders vulnerable. Additionally, inflammation can damage the protective barriers in your respiratory tract, giving pathogens easier access.
Many people notice that when they address their underlying inflammatory triggers, not only do they get sick less frequently, but when they do catch something, their recovery time shortens dramatically. Your susceptibility to common infections often reflects your overall inflammatory burden.
15. Worsening Seasonal Allergies

Your once-mild spring sniffles have escalated to full-blown seasonal misery. This intensification of allergic responses often signals that your immune system is in an inflammation-primed state year-round, not just during pollen season.
When your body is already dealing with chronic inflammation, your mast cells and other immune components become hyper-responsive to triggers they previously tolerated. The threshold for reaction lowers dramatically. Many people describe it as their “allergy cup” being already nearly full from existing inflammation, so even small amounts of pollen or other allergens cause it to overflow.
Addressing baseline inflammation often reduces seasonal suffering more effectively than antihistamines alone. People frequently report needing less allergy medication after reducing their overall inflammatory load through dietary and lifestyle changes.
16. Menstrual Changes or Worsening PMS

Your periods have become more painful, irregular, or accompanied by more intense emotional symptoms. These menstrual changes often indicate that inflammation is interfering with your hormonal balance and signaling pathways. Inflammatory compounds can directly impact your endocrine system, particularly affecting estrogen metabolism and progesterone sensitivity.
The inflammation can also trigger increased production of prostaglandins—hormone-like substances that cause the uterus to contract more intensely. Many women experience these changes as more severe cramps, heavier bleeding, or emotional symptoms that seem disproportionate.
While hormonal fluctuations are normal, dramatic worsening of period-related symptoms often reflects underlying inflammatory processes. Addressing inflammation frequently improves cycle regularity and reduces symptom severity more effectively than hormonal interventions alone.
17. Decreased Libido Without Explanation

Your interest in sex has diminished without any relationship changes or obvious causes. This unexplained drop in libido often signals that inflammation is affecting your hormonal production and stress response systems. Chronic inflammation directly impacts testosterone levels in all genders, not just men.
It also increases cortisol production, which further suppresses sex hormone production. The inflammatory process can also affect blood flow to genital tissues and dampen the neural pathways involved in arousal. Many people mistakenly attribute decreased libido solely to aging, stress, or relationship issues.
While these factors certainly matter, addressing underlying inflammation often restores sexual interest more effectively than relationship interventions or supplements alone. Your body wisely conserves reproductive energy when it detects potential threats via inflammatory signals.
18. Body Odor Changes Despite Good Hygiene

Your natural scent has changed in ways that regular showering doesn’t fix. This altered body odor often indicates that inflammation is changing your metabolic processes and affecting your microbiome composition. When inflammation disrupts your normal metabolism, your body produces different waste compounds that are excreted through sweat and breath.
These metabolic byproducts often have a more sour, ammonia-like, or metallic quality compared to your normal scent. Additionally, inflammation can alter the balance of bacteria living on your skin, which significantly impacts body odor.
Many people mistakenly address this symptom with stronger antiperspirants or deodorants rather than investigating the root cause. The distinctive smell—often noticed first thing in the morning or during stress—can be an early warning sign of metabolic inflammation worth paying attention to.
19. New or More Frequent Headaches

Headaches have become your unwelcome companion, appearing without obvious triggers. These unexplained head pains often signal vascular inflammation or increased sensitivity to inflammatory compounds like histamine.
When blood vessels in and around your brain become inflamed, they can dilate or constrict abnormally, triggering pain signals. Inflammation also sensitizes your nervous system, lowering the threshold at which normal stimuli become painful. Many people describe these inflammation-related headaches as feeling different from their usual tension headaches—often with a throbbing quality or accompanied by sensitivity to light or sound.
The timing of these headaches frequently correlates with inflammatory exposures, particularly certain foods, environmental triggers, or stress. Keeping a detailed headache journal often reveals patterns connecting inflammatory triggers to head pain that simple pain relievers don’t address effectively.
20. Unusual Temperature Sensitivity

You’re suddenly always too hot or constantly freezing when everyone else is comfortable. This disrupted temperature regulation often indicates that inflammation is affecting your autonomic nervous system and hypothalamus function. Your internal thermostat, located in the hypothalamus of your brain, can be directly influenced by inflammatory cytokines.
This disruption leads to inappropriate vasodilation (feeling flushed or hot) or vasoconstriction (feeling chilled) regardless of the actual environmental temperature. Many people also notice increased sweating, particularly night sweats that aren’t explained by room temperature or bedding.
These temperature regulation issues often fluctuate with inflammatory flares, providing a useful tracking mechanism. If you find yourself constantly adjusting the thermostat or dressing in layers while others remain comfortable, consider investigating inflammatory triggers rather than just blaming the weather.
21. Unexplained Weight Changes

Your weight fluctuates without changes to your diet or exercise routine. These mysterious shifts—either gains or losses—often signal that inflammation is affecting your metabolism and hormone signaling. When inflammation becomes chronic, it can disrupt your body’s normal hunger and satiety signals, leading to unintentional overeating or appetite suppression.
Inflammatory cytokines also directly impact your thyroid function, potentially slowing your metabolic rate. Additionally, inflammation affects how your body stores and uses fat, potentially causing weight gain even with calorie control.
The weight changes associated with inflammation tend to have a different pattern than those from simple caloric imbalance—they often appear relatively suddenly and don’t respond predictably to dietary adjustments. Many people find that addressing inflammation helps normalize their weight more effectively than calorie-focused approaches alone.

Comments
Loading…